Top 10 Gynecologists in Alwarpet, Chennai

Introduction Alwarpet is one of Chennai’s most sought-after residential localities, known for its premium neighbourhoods, calm surroundings, and proximity to quality healthcare institutions. Women living in Alwarpet often look for gynecologists who offer a balance of medical expertise, privacy, comfort, and personalised attention. From routine gynecological consultations and pregnancy care to fertility treatment and long-term […]
Top 10 Gynecologist in Teynampet, Chennai

Introduction Teynampet is a centrally located neighbourhood in Chennai, positioned along Anna Salai and well connected to areas like Nandanam, Thousand Lights, and Nungambakkam. Because of its excellent accessibility and proximity to reputed hospitals and clinics, many women prefer Teynampet for gynecology, maternity, fertility, and reproductive healthcare. From routine gynecological check-ups to pregnancy care and […]
Top 10 Gynecologists in T. Nagar, Chennai

Introduction Selecting the right gynecologist is essential for women seeking comprehensive healthcare and a comfortable pregnancy experience. T. Nagar, Chennai, hosts a range of reputable clinics offering advanced gynecology, maternity, and fertility services. From routine check-ups to specialized treatments, choosing the right expert ensures safety, personalized attention, and peace of mind. In this guide, we […]
Top 10 Gynecologists in Choolaimedu, Chennai

Introduction Choosing the right gynecologist in Choolaimedu is essential for a safe, healthy, and comfortable experience, whether it’s for routine check-ups, fertility guidance, or pregnancy care. The right specialist can make all the difference in your overall women’s wellness journey. Choolaimedu has several clinics and hospital departments that provide women’s health services. This guide lists […]
Top 10 Gynecologists in Anna Nagar

Introduction Anna Nagar is one of Chennai’s most well-planned residential neighborhoods, offering easy access to quality healthcare facilities. For women seeking gynecology, maternity, fertility, or reproductive health care, choosing the right doctor inby is crucial. Whether it’s routine check-ups, prenatal care, fertility guidance, or advanced OB-GYN treatments, having a trusted clinic makes a big difference. […]
Top 10 Gynecologist in Mount Road, Chennai
Introduction Mount Road (Anna Salai) is one of Chennai’s most prominent healthcare corridors, connecting key localities such as Teynampet, Thousand Lights, Egmore, and Nungambakkam. Thanks to its central location and excellent accessibility, many women prefer Mount Road when seeking gynecology, maternity, fertility, and reproductive healthcare services. From routine gynecological consultations to advanced pregnancy care and […]
Top 10 Gynecologists in Vadapalani, Chennai

Introduction Vadapalani is a bustling residential and commercial area in Chennai, known for its connectivity and access to quality healthcare services. Women in Vadapalani seeking gynecology, maternity, fertility, or reproductive health care require trusted doctors who combine expertise with personalized attention. From routine gynecological check-ups to advanced maternity care and fertility treatments, selecting the right […]
Top 10 Gynecologists in Kodambakkam, Chennai

Introduction Women’s health is an integral part of overall wellbeing, and choosing the right gynecologist can have a profound impact on reproductive health, pregnancy care, and long-term wellness. Whether it’s for routine check-ups, fertility guidance, menstrual concerns, PCOS, or advanced maternity care, having a trusted specialist ensures peace of mind and safe care. Kodambakkam, along […]
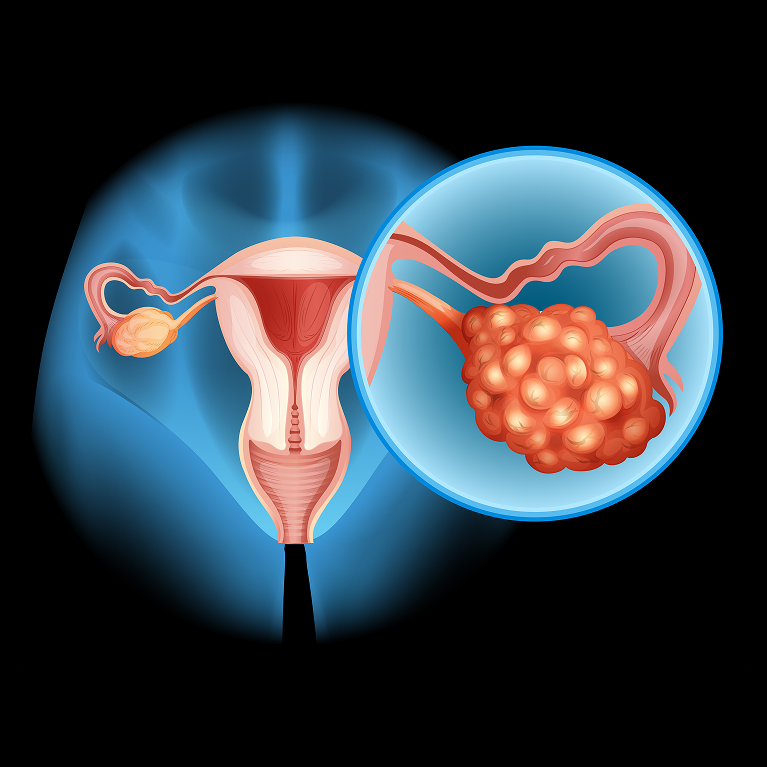
Pap Smears: The Importance of Cervical Health Screening

When it comes to women’s preventive healthcare, few tests are as powerful and life-saving as pap smears. This simple screening test has dramatically reduced cervical cancer deaths worldwide by detecting early cellular changes before they become dangerous. Yet many women still delay or avoid pap smears because of fear, embarrassment, lack of awareness, or the […]
Menopause Symptoms and Causes: Signs Every Woman Should Know
It happens because the ovaries gradually reduce their production of the hormones estrogen and progesterone, which regulate the menstrual cycle and affect many systems in the body.Each stage plays a role in shaping the menopause symptoms and causes experienced by different women. The transition into menopause occurs in three stages: Perimenopause – The years leading […]
