How to Prepare for Your First Mammogram Visit | Complete Guide

For many women, a Mammogram Visit can feel intimidating—especially if it’s your first one. Questions about discomfort, results, preparation, and anxiety are completely normal. The good news? With the right information, your Mammogram Visit can be smooth, quick, and empowering. A mammogram is a vital screening tool that helps detect breast changes early, often before […]
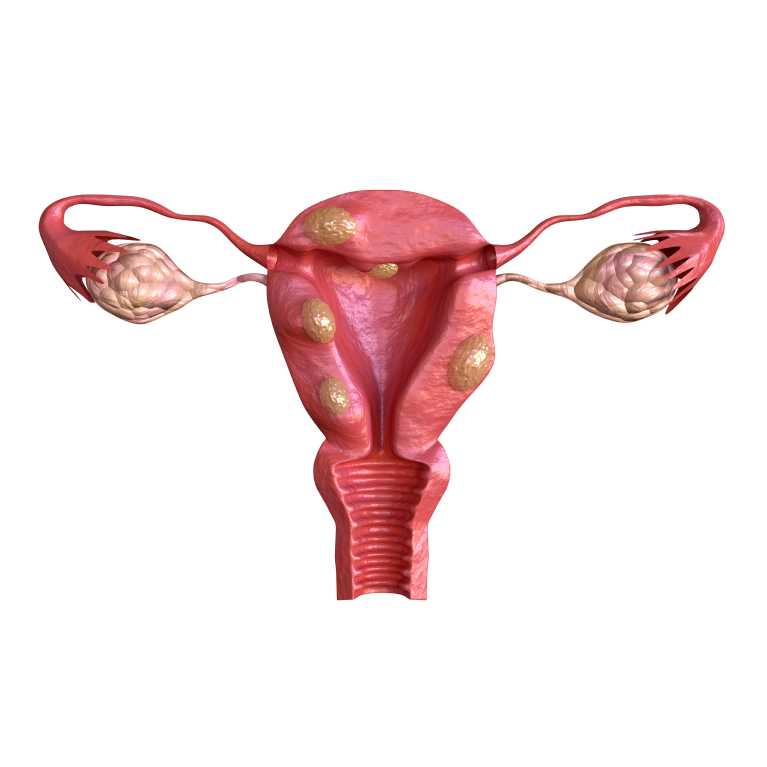
The Silent Signs of Fibroids: What Every Woman Should Know
Uterine fibroids are harmless growths in the uterus that many women may not even realize they have. While they are incredibly common—affecting up to 70% of women by age 50—they often go unnoticed until they cause more serious symptoms. This makes understanding the silent signs of fibroids essential for women of all ages. By recognizing […]
Understanding the Importance of Anomaly Scans During Pregnancy

Pregnancy is a journey filled with excitement, anticipation, and many important medical check-ups that ensure the well-being of both mother and baby. One of the most crucial investigations during pregnancy is the anomaly scan, commonly known as the 20 week screening scan. This detailed ultrasound plays a vital role in assessing the baby’s development and […]
Living with Endometriosis? Symptoms & Life-Changing Treatments Explained
Living with chronic pain that often goes unseen can be emotionally and physically exhausting. For millions of women worldwide, living with endometriosis , causes and symptoms is a daily reality that affects work, relationships, mental health, and overall quality of life. Despite being common, endometriosis is frequently misunderstood, misdiagnosed, or ignored. This blog explains what […]
Best Gynaecologist for PCOS | PCOD treatment in Chennai

PCOS is one of the most common hormonal disorders affecting women today, but the journey to diagnosis and healing can feel overwhelming. With symptoms like irregular periods, acne, weight gain, fertility struggles, and hair thinning, finding the best doctor for PCOS treatment becomes crucial. The right specialist not only diagnoses PCOS accurately but also guides […]
Top Tips for a Painless Delivery | Expert Guide for Expecting Moms

Every mother dreams of a smooth, comfortable, and painless delivery—a birth experience where fear is replaced with confidence and excitement. While pain is a natural part of childbirth, modern techniques, the right mindset, and timely medical support can significantly reduce discomfort and make labor easier. This guide reveals expert-approved strategies to help you achieve a […]
Third Trimester Pregnancy: Essential Care Tips for a Healthy Delivery

The third trimester pregnancy phase is an exciting, transformative, and sometimes overwhelming journey for every expecting mother. As you enter the final stretch—from week 28 to week 40—your body prepares intensely for childbirth. Your baby grows rapidly, your organs shift to make space, and you may experience physical and emotional changes that require mindful care. […]
Top IVF & Gynecology Clinic in Nungambakkam, Chennai
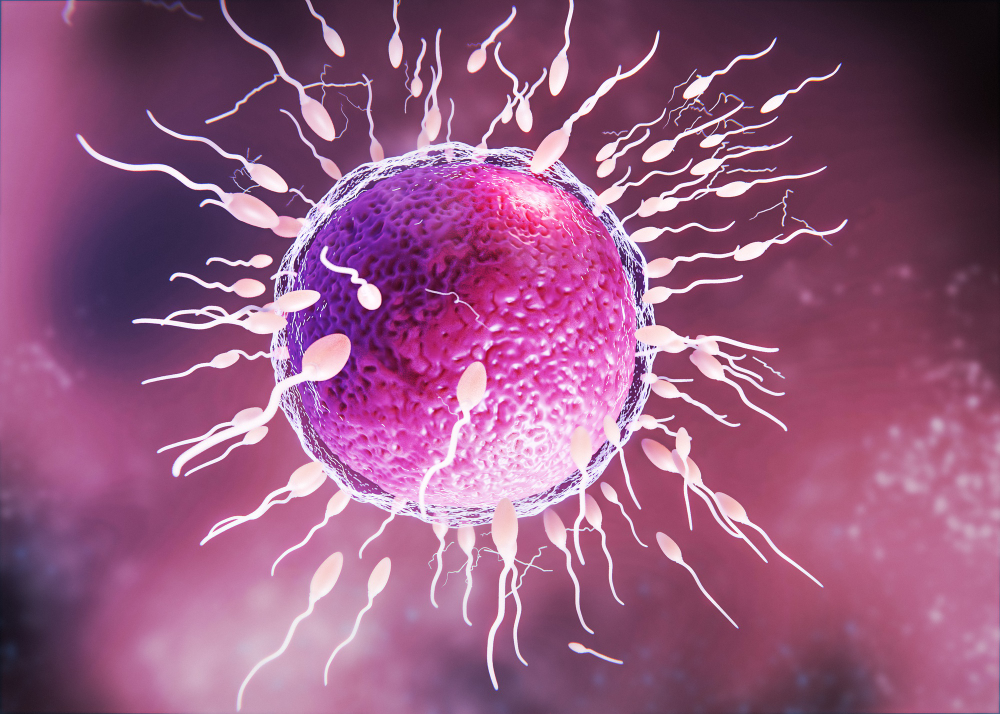
Starting a family is one of life’s most beautiful journeys, but for many couples, challenges like infertility can make this dream feel distant. Fortunately, with advancements in reproductive medicine, hope is within reach. If you are seeking exceptional care in Chennai, a top IVF clinic can provide the expertise, technology, and compassionate support you need […]
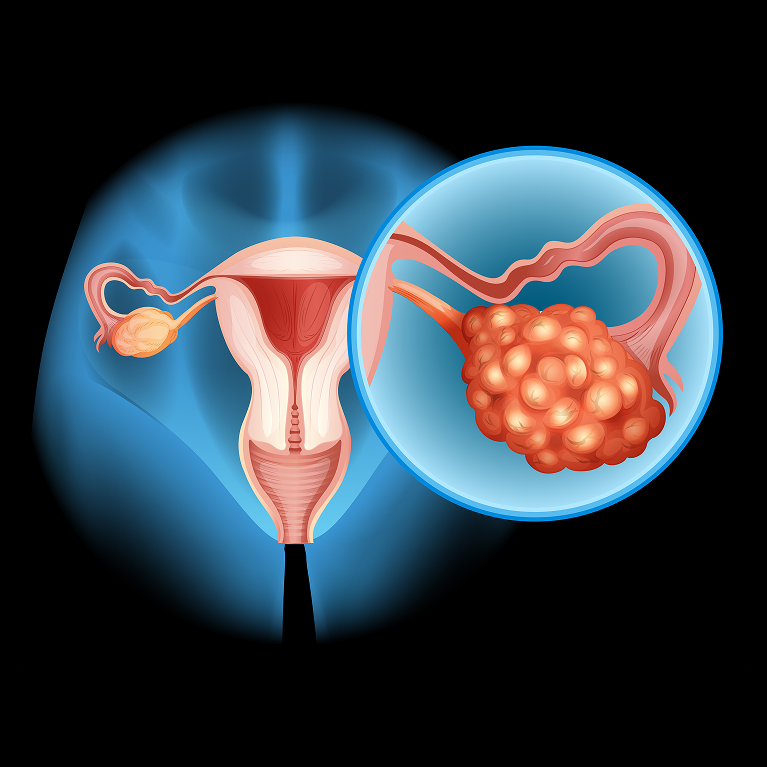
What is the Ideal Treatment for Endometriosis Ovarian Cyst?

Endometriosis is one of the most commonly underdiagnosed gynaecological conditions in women, especially when it forms ovarian cysts, also known as endometriomas or “chocolate cysts.” These cysts can cause severe pain, heavy periods, fertility difficulties, bloating, and chronic pelvic discomfort. When it comes to finding the ideal Endometriosis diagonisis treatment, there is no “one-size-fits-all” approach. […]
Safe & Effective Methods for Vaginal Health

Many women search for ways to tighten your vagina naturally, especially after childbirth, hormonal changes, or aging. It’s important to understand that the vagina itself doesn’t “loosen” permanently – but the pelvic floor muscles supporting it may weaken over time. When these muscles lose strength, you may experience reduced sensation, mild urine leakage (incontinence), or […]
